Physician Team

Why Personal Cell Therapy?
We obtain high numbers of these viable cells and we are studying the conditions that respond best, at which time points, and which deployment methods are most effective by following up with all of our patients for a 5 year period post-therapy. This effort, which has been underway for over 10 years now, has led us to publish over 10 peer-reviewed publications, the largest of their respective kind, documenting safety and efficacy in a number of different clinical areas as well as teaching over 500 physicians across the USA and around the globe our techniques for their own implementation. The California Stem Cell Treatment Center employs a clinical research coordinator to continuously analyze our valuable data and our vision is to perfect our treatments and ultimately teach them to other physicians around the world.
Frequently Asked Questions
Our own Dr. Mark Berman, of the California Stem Cell Treatment Center, is featured in Episode 4. To learn about this important film, click here. If you have additional questions on how stem cells work and how they relate to your condition, contact us today to schedule your free, no-obligation consultation. To get the process started, simply fill out our short Confidential Candidate Application.
What is a stem cell?
A stem cell is basically any cell that heal other cells and tissues. Stem cells can both replicate to duplicate itself and also differentiate (form other cells and tissues upon demand). A commonly heard term is “adult” stem cell. These are stem cells that come from umbilical tissue, bone marrow or fat.
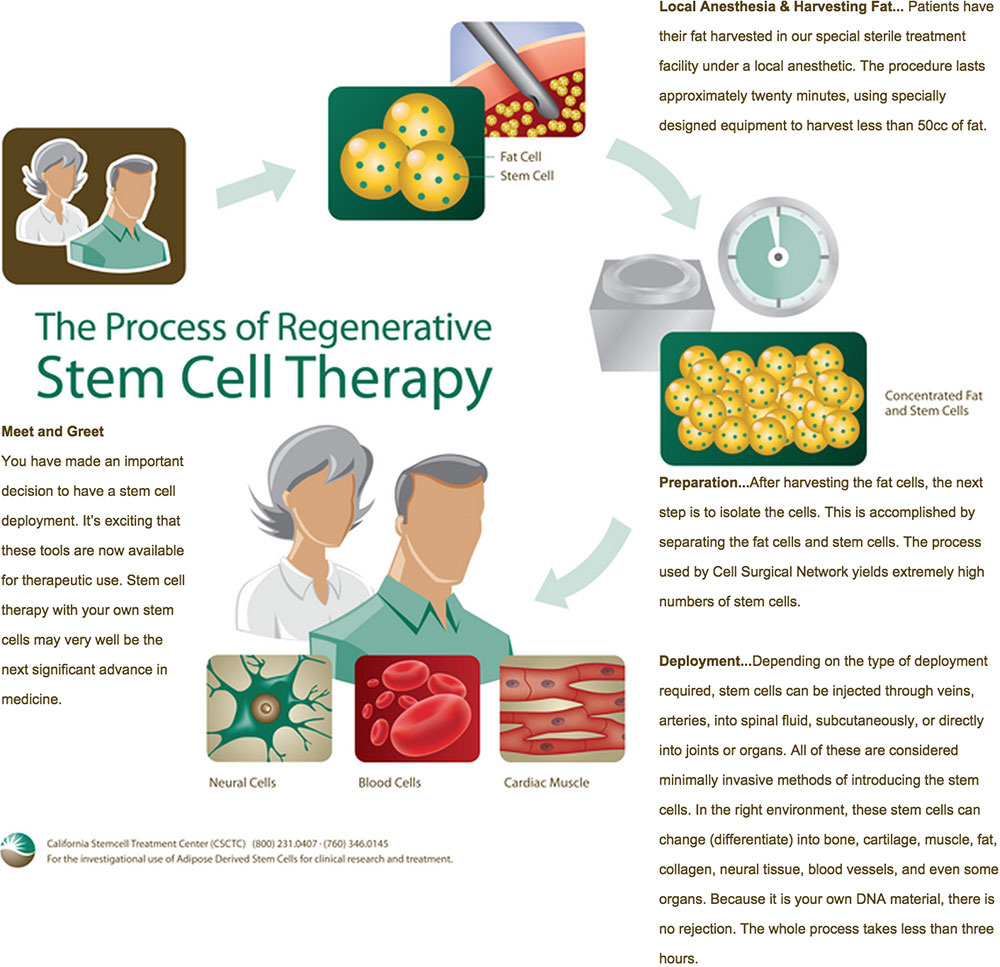
Why Use Fat? The California Stem Cell Treatment center’s cell harvesting and isolation techniques are based on technology from South Korea. We use adipose (fat) derived stem cells for investigational clinical treatments Early stem cell research has traditionally been associated with the controversial use of embryonic stem cells. The new focus is on non-embryonic adult mesenchymal stem cells which are found in a person’s own blood, bone marrow, and fat. Cell therapy around the world is shifting its focus from bone marrow based cells to adipose (fat) derived cells since the cells are easy to obtain and generally very robust. Adipose fat is an abundant and reliable source of stem cells. The best quality adipose stem cells are derived from the enzymatic digestion of lipo-suctioned fat which can be performed at the bedside in a closed system to protect sterility. Autologous stem cells from a person’s own fat are easy to harvest safely under local anesthesia and are abundant in quantities up to 1000 times those seen in bone marrow. Fat derived stem cells have the same telomere length (cellular age) as umbilical stem cells for the first four decades of life, but consistently remain younger than bone marrow stem cells at any chronologic age. The fat derived cells also grow in culture and differentiate faster than the bone marrow derived stem cells that are commonly used.
What is Regenerative Medicine?
Regenerative Medicine is the process of creating living, functional tissues to repair or replace tissue or organ function lost due to damage, or congenital defects. This field holds the promise of regenerating damaged tissues and organs in the body by stimulating previously irreparable organs to heal themselves.
What are the tools of Regenerative Medicine?
Traditionally, we have used various medications and hormones to limit disease and help the body repair itself. For example, hormone replacement therapy has, in many cases, shown the ability to more optimally help the immune system and thus help us repair diseased or injured tissues. Genetic research is an evolving area where we will eventually learn and utilize more ways of specifically dealing with gene defects causing degenerative disease. Stem cell therapy has already shown considerable promise in alleviating many degenerative conditions. Stem cells communicate with our tissues to provide regenerative and healing signals through a complex signaling system mediated by exosomes (containing genetic material) and also peptide cytokines or “growth factors,” which can promote regeneration.
How do stem cells heal?
Stem cells are found all over the body but they remain dormant unless they interact with some level of cellular injury. It’s the injury signals like beacons that attract stem cells and turns them on to start the healing process. So, when a person has a degenerative type problem, the stem cells tend to go to that area of need and stimulate the healing process. Stem cells can promote healing by either directly differentiating into target cells and functional tissue or by proxy healing which is based on secretion of growth factors and exosomes that signal for repair and regeneration of other cells, Stem cells can even transfer their healthy “power pack” mitochondria (energy producing organelle in all your cells) to aging or dying cells in your body.
Are the stem cell treatments at California Stem Cell approved by the FDA?
No, The California Stem Cell Treatment Center’s surgical procedures fall under the category of physician’s practice of medicine, wherein the physician and patient are free to consider their chosen course of treatment. The FDA does have guidelines governing use of a patient’s own tissues. At the California Stem Cell Treatment Center, we meet certain FDA requirements by providing the “same surgical procedure” exclusion using a patient’s own cells that undergo no manipulation and are deployed during the same procedure.
Does California Stem Cell provide patient testimonials?
Many patients have heard compelling testimonials about stem cells in the through marketing website, brochures, and on various websites where one can read about remarkable results of stem cell treatments. California Stem Cell does not believe in such marketing claims or testimonials since our work is still investigational. Nevertheless, we are data driven and we are a resource for patients who need access to regenerative care. California Stem Cell gives a choice to those informed patients who seek modern regenerative therapy but desire convenience, quality and affordability.
Is it better to use umbilical stem cells since they may be younger than your own?
The umbilical cells can be slightly younger than the stem cells of a middle aged person but that is not worth the negative factors of receiving cells that are not made out of your own DNA. When you use your own stem cells, there is no risk of transmissible disease contamination and there is no risk of allergic reaction or immune reaction.
Can stem cells from fat cause cancer?
Adult mesenchymal stem cells are not known to cause cancer. Some patients have heard of stories of cancer caused by stem cells, but these are probably related to the use of embryonic cells (Not adult stem cells). These embryonic tumors known as teratomas are rare but possible occurrences when embryonic cells are used. California Stem Cell does not use embryonic stem cells under any conditions.
Are there reports of stem cells causing harm to recipients?
The California Stem Cell Treatment Center uses a sophisticated database to follow all our outcomes and any adverse events and we have had extraordinary safety since we started treating patients in 2010.
Is radiology technology required to administer a person’s stem cells?
California Stem Cell has both ultrasound and fluoroscopy technology at our facility and these modalities are used for many complex stem cell injections for complete targeting accuracy.
How long does it take to see improvement?
Stem cell therapy relies on the body’s own regenerative healing to occur. The regenerative process may take time, particularly with orthopedic patients, who may not see results for several months. In some diseases, more immediate responses are possible.
Is everyone a candidate?
No. Only certain medical problems are currently being treated at the California Stem Cell Treatment Center. Check our list or fill out a candidate application form on the website. All patients need to be medically stable enough to have the treatment in our facility. Some patients may be declined due to the complexity of their problem. Other patients may not have conditions appropriate to treat or may not be covered by our specialists or our protocols. An outside referral (if we know of someone else treating such a problem) might be applicable in such cases.
How many treatments are required for a favorable conical outcome?
Most patients, especially those with orthopedic conditions, require only one deployment. Certain types of degenerative conditions, particularly auto-immune disease or neuro-degenerative disorders, may respond best to a series of stem cell deployments. The number and necessity of any additional treatments would be decided on a case by case basis.
What is the cost of consultation and treatment?
Patients who are considered to be candidates for our protocols may be offered a complimentary consultation. Unfortunately, insurance generally will not cover the actual cost of our stem cell treatments since stem cell therapy is still considered investigational. The ultimate cost varies depending on the disease state being treated and which type of stem cell deployment is required. Because of recent innovations in technology, the California Stem Cell Treatment Center is able to provide outpatient stem cell treatment at a fraction of the cost of that seen in many overseas clinics. Our fees cover Stromal Vascular Fraction SVF harvesting, preparation, and deployment which may include the use of advanced interventional radiology and fluoroscopy techniques. Total costs will be determined after a medical evaluation.




 Mark Berman, MD, is an internationally renowned expert in the field of regenerative medicine and cellular therapy and helped to restore the health of thousands of patients around the globe – without dangerous prescription drugs or risky surgery.
Mark Berman, MD, is an internationally renowned expert in the field of regenerative medicine and cellular therapy and helped to restore the health of thousands of patients around the globe – without dangerous prescription drugs or risky surgery. Dr. Elliot Lander, a Board-Certified Urologist, is Co-Founder and Co-Medical Director of
Dr. Elliot Lander, a Board-Certified Urologist, is Co-Founder and Co-Medical Director of  Dr. Grogan is a practicing pediatric orthopedic surgeon at Pacific Coast Sports Medicine in Los Angeles. Dr. Grogan graduated cum laude from Princeton University with a degree in Biology and received his medical degree from the University of Cincinnati College of Medicine. Dr. Grogan’s orthopedic training has included an orthopedic residency at UCLA plus several orthopedic fellowships in pediatric orthopedics, trauma, and NIH sponsored joint replacement surgery. Following his orthopedic training he returned to Los Angeles, spending six years at Shriner’s Hospital for Crippled Children, including serving as Assistant Chief in 1996 and 1997. In addition to his clinical practice, he spent several years involved in managed care consulting as an orthopedic surgeon and has developed special expertise in this area. He has collaborated with the American Academy of Orthopedic Surgeons in the development of a handbook and audiotape entitled, “Health Care Reform and Managed Care: A Guidebook for Orthopedic Surgeons”. In addition, he has served as the lead faculty member for the AAOS for their 1995, 12 city educational seminar, “Taking Charge: Managed Care Contracting for Orthopedic Surgeons” and as a faculty member for the AAOS’s 1996 seminar series entitled, “Winning at Risk: The Interplay of Cost, Quality, and Access in Orthopedic Practice”. He most recently served as a faculty member for the AAOS’s 2009, 2010, 2011 and 2012 seminars, “Practice Management Symposium for Practicing Orthopedic Surgeons’. He is currently chairman of the Practice Management Committee for the American Academy of Orthopedic Surgeons and a member of their Council on Education. He is a member of Alpha Omega Alpha, Honor Medical Society, the Sigma XI Scientific Research Society, California Orthopedic Association (COA), the Pediatric Orthopedic Society of North America (POSNA), the American Academy of Orthopedic Surgeons (AAOS), and is a diplomate of the American Board of Orthopedic Surgery.
Dr. Grogan is a practicing pediatric orthopedic surgeon at Pacific Coast Sports Medicine in Los Angeles. Dr. Grogan graduated cum laude from Princeton University with a degree in Biology and received his medical degree from the University of Cincinnati College of Medicine. Dr. Grogan’s orthopedic training has included an orthopedic residency at UCLA plus several orthopedic fellowships in pediatric orthopedics, trauma, and NIH sponsored joint replacement surgery. Following his orthopedic training he returned to Los Angeles, spending six years at Shriner’s Hospital for Crippled Children, including serving as Assistant Chief in 1996 and 1997. In addition to his clinical practice, he spent several years involved in managed care consulting as an orthopedic surgeon and has developed special expertise in this area. He has collaborated with the American Academy of Orthopedic Surgeons in the development of a handbook and audiotape entitled, “Health Care Reform and Managed Care: A Guidebook for Orthopedic Surgeons”. In addition, he has served as the lead faculty member for the AAOS for their 1995, 12 city educational seminar, “Taking Charge: Managed Care Contracting for Orthopedic Surgeons” and as a faculty member for the AAOS’s 1996 seminar series entitled, “Winning at Risk: The Interplay of Cost, Quality, and Access in Orthopedic Practice”. He most recently served as a faculty member for the AAOS’s 2009, 2010, 2011 and 2012 seminars, “Practice Management Symposium for Practicing Orthopedic Surgeons’. He is currently chairman of the Practice Management Committee for the American Academy of Orthopedic Surgeons and a member of their Council on Education. He is a member of Alpha Omega Alpha, Honor Medical Society, the Sigma XI Scientific Research Society, California Orthopedic Association (COA), the Pediatric Orthopedic Society of North America (POSNA), the American Academy of Orthopedic Surgeons (AAOS), and is a diplomate of the American Board of Orthopedic Surgery.