What is Interstitial Cystitis?
Interstitial cystitis (in-tur-STISH-ul sis-TIE-tis) is a chronic condition causing bladder pressure, bladder pain and sometimes pelvic pain.
The pain ranges from mild discomfort to extremely intense pain. IC is a part of a spectrum of diseases known as painful bladder syndrome.
Your bladder is a hollow, muscular organ that stores urine.
The bladder expands until it’s full and then signals your brain that it’s time to urinate, communicating through the pelvic nerves. This creates the urge to urinate for most people.
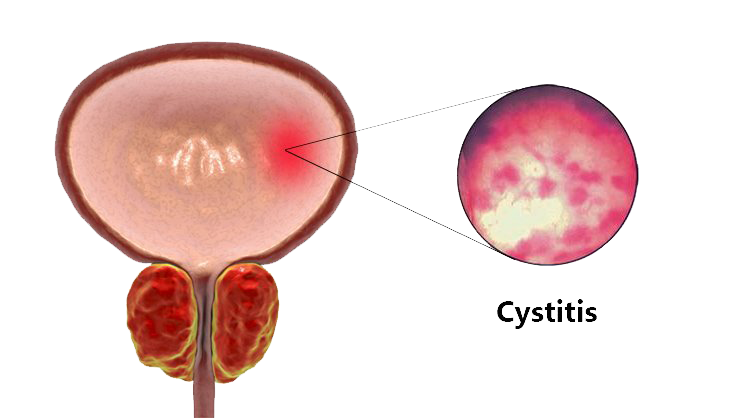
Your bladder, kidneys, ureters and urethra make up your urinary system. When you have interstitial cystitis, the walls of your bladder become irritated and inflamed, compared with those of a normal bladder.
With interstitial cystitis, these signals get mixed up — you feel the need to urinate more often and with smaller volumes of urine than most people.
Interstitial cystitis most often affects women and can have a long-lasting impact on quality of life.
Although there’s no cure, medications, an altered diet and other therapies may offer relief.
Is Interstitial Cystitis related to other inflammatory conditions?
This condition involves the inflammation and irritation of the bladder walls, which results in abnormal signals being sent to the brain, causing a frequent urge to urinate with smaller volumes of urine.
It primarily affects women and can have a significant and enduring effect on their quality of life.
While there is no cure for interstitial cystitis, there are various medications and therapies available that can provide relief.
The IC diet has also shown to be quite effective at managing flare-ups.